In this article, we will discuss what Thalassemia how is it diagnosed and treated.
Thalassemia is an inheritable blood disorder that impacts the body’s ability to make hemoglobin and healthy red blood cells. There are two kinds of Thalassemia.
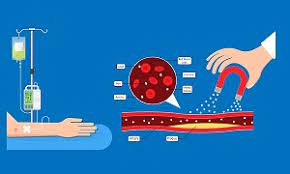
Thalassemia can cause anemia-like symptoms ranging from mild to extreme. Treatment options include blood transfusions as well as iron treatment with chelation.
What is Thalassemia?
Thalassemia (thal-uh-SEE-me-uh) is an inheritable blood disorder that is inherited.
It interferes with your body’s ability to make normal hemoglobin. Hemoglobin is the protein found in red blood cells.
It allows red blood cells to move oxygen around your body while also nourishing the cells of your body.
If you suffer from Thalassemia, your body produces less healthy hemoglobin protein, and your bone marrow can produce less healthy red blood cells.
Having fewer red blood cells can be referred to as anemia.
Since red blood cells play essential functions in delivering oxygen to tissues within your body, having sufficient healthful red blood cells could cause your body’s cells to be deficient in the oxygen they require to produce energy and grow.
Symptoms of Thalassemia
Thalassemia symptoms may vary. The most frequent symptoms are:
Bone deformities are common, particularly in the face.
Dark urine
Retarded expansion and development
Excessive fatigue along with fatigue
Pale or yellow skin
There are not all people who show visible signs of Thalassemia. The signs of the disorder are more common in adolescence or childhood.
Causes of Thalassemia
The hemoglobin protein transports oxygen throughout the body through blood cells.
Bone marrow uses iron that people get from food to produce hemoglobin.
For those suffering from Thalassemia, the bone marrow fails to produce sufficient healthy hemoglobin, also known as red blood cells.
The body also breaks down red blood cells by using abnormal hemoglobin.
Furthermore, these red blood cells might not be able to pass through capillaries to access the essential parts of the body.
In certain instances, this could cause a deficiency of oxygen, which can cause anemia and fatigue.
Thalassemia sufferers with mild cases might not require treatment; however, more severe cases may require regularly scheduled blood transfusions.
How is Thalassemia diagnosed?
Most children suffering from mild to extreme Thalassemia get an early diagnosis when they reach the age of 2.
Patients with no symptoms might not be aware that they have a condition until they are parents of children with Thalassemia.
Blood tests can tell the presence of the thalassemia carrier or suffers from the disorder.
These are the methods of testing doctors employ to make the diagnosis:
Total blood count (CBC): This allows you to measure hemoglobin levels and the size and level of red blood cells.
A reticulocyte count measures the rapid reticulocytes, also known as mature red blood cells, released and produced from bone marrow.
Reticulocytes typically last for 2 days in the bloodstream before maturing into mature red blood cells.
About 1 to 2 percent of a healthy individual’s red blood cells are reticulocytes.
Iron levels will help doctors determine the source of anemia and whether it is due to Thalassemia or iron deficiency.
When it comes to Thalassemia, iron deficiency is not the reason for the condition.
Genetic tests: DNA analysis will reveal if someone has Thalassemia or genetic mutations.
Prenatal tests can determine if the fetus has Thalassemia and how severe it could be.
Chorionic villus sample (CVS): A portion of the placenta is removed to be tested, typically around the 11th week of pregnancy.
Amniocentesis Healthcare professionals collect an insignificant amount of amniotic fluid to be tested, usually at the 16th-week pregnancy. Amniotic fluid refers to the fluid which covers the
What are the types of Thalassemia?
Thalassemia is considered a trait minor, intermedia, and major to indicate how severe the condition is.
These classifications represent a range that a thalassemia complication can mean that you will have mild anemia symptoms or none whatsoever.
It is possible that you do not require treatment. Thalassemia major can be the most severe form and typically needs regular care.
There are two kinds of Thalassemia, beta thalassemia, and alpha — named for problems within this chain.
Alpha Thalassemia
You have four genes in your family, two of each parent, creating proteins called alpha-globin.
If any of the genes are deficient, the result is that you get alpha Thalassemia.
The number of genes you carry that are defective will determine if you suffer from anemia symptoms and (if this is the case) how severe they’ll be.
A deficient or absent alpha gene is that you won’t be able to experience any symptoms. Another term for this condition is alpha thalassemia minimal.
Two deficient or missing Alpha genes imply that it’ll probably be minimal if you suffer from symptoms. Another term is alpha thalassemia minor.
Three defective or missing alpha genes signify that you’ll be experiencing mild or severe signs.
Another term for this disorder is Hemoglobin H disease.
The presence of four defective or missing alpha genes typically leads to the death of a baby.
In the rare cases that the baby can survive, they’ll probably require life-long blood transfusions. Another name for this problem is hydrops fetalis, which includes Hemoglobin Barts.
Beta Thalassemia
The beta-globin gene is inherited by two people, two genes in each of your parents.
The severity of your anemia and the symptoms you experience, as well as the severity of your condition, depend on how many genes are affected and which segment of the beta-globin chain of proteins has the defect.
A defective or missing beta gene
Signifies that you’ll suffer minor symptoms. Another name for this disorder is beta Thalassemia Minor.
Two missing or defective beta genes
Can cause mild or severe signs. The mild variant is known as Thalassemia intermediate.
A more severe form of beta thalassemia with the two gene mutations is known as beta-thalassemia major, also known as Cooley’s anemia.
Treatment of Thalassemia
Treatment is dependent on the type and the severity of Thalassemia.
Transfusions of blood:
These can replenish hemoglobin and red blood cell levels. Thalassemia patients will require between 8 to 12 transfusions per year.
Those with less severe Thalassemia may require up to eight transfusions per year or more during stress or illness. Infections.
Iron Chelation:
This process involves the removal of excess iron from the bloodstream. The transfusion of blood may result in iron over-production.
This could cause damage to the heart as well as other organs. Doctors might prescribe deferoxamine.
An injection drug that is administered through the skin or into the muscle. They may also prescribe deferasirox, which is taken by mouth.
Supplementation with folic acid:
People who receive blood transfusions and chelation could require Folic acid supplements. They help red blood cells to grow.
Bone marrow or stem cells, transplants:
Bone marrow cells produce white and red hemoglobin, blood cells, and platelets. In extreme situations, a transplant of a compatible donor could be a successful treatment.
Operation:
This may be needed to correct bone irregularities.
Gene therapy:
Researchers are studying ways to use gene therapy to combat Thalassemia. Possible options include inserting the beta-globin gene of normality into a patient’s bone marrow or using medications to activate the genes responsible for the fetal hemoglobin.
FAQ about What is Thalassemia, how is it diagnosed and treated
Can the thalassemia virus be prevented?
Thalassemia isn’t preventable; however, genetic testing may determine if you or your spouse carry the gene. Knowing this information will assist you in planning your pregnancy if you are planning to get pregnant.
Talk to an experienced genetic counselor for guidance regarding family planning if you think you or your partner could be carriers of gene mutations for Thalassemia.
Can Thalassemia be treated?
The bone marrow donation by an identical sibling is the greatest chance of a cure for Thalassemia. However, most patients with Thalassemia do not have a donor sibling. Furthermore, a bone-marrow transplant is a risky procedure that can result in serious complications and lead to death.
Consult a specialist in Thalassemia to determine if you’re a candidate for a donor. Selecting a hospital with a large volume that regularly performs bone marrow transplants increases the chance of receiving a cure while also reducing the chances of suffering from complications.
What is the average life expectancy of a person with Thalassemia?
It is normal to have a life expectancy for those with mild Thalassemia. Even if the disease is severe or moderate, there is a high chance of surviving long-term if you adhere to the treatment plan (transfusions and iron treatment with chelation).
Heart disease caused by over-excitability to iron is the primary cause of death among patients with Thalassemia. Therefore maintaining the iron chelation treatment is crucial.

